Several factors could potentially account for the co-occurrence of constipation and PCOS in females. To begin with, one contributing factor is irritable bowel syndrome (IBS), a gastrointestinal disorder characterized by distressing digestive symptoms such as diarrhea, constipation, or a combination of both. It is noteworthy that IBS, particularly the subtype associated with constipation, is more prevalent among women with PCOS.
Another factor worth considering is dysbiosis, an imbalance of gut bacteria, which may be responsible for the heightened incidence of constipation among women with PCOS. Dysbiosis arises when there is an overabundance of harmful bacteria, a deficiency of beneficial bacteria, or an insufficient diversity of bacterial species in the gut. Women with PCOS are more prone to experiencing gut dysbiosis compared to those without the condition.
Additionally, in certain individuals, constipation may be attributed to small intestinal bacterial overgrowth (SIBO), a type of dysbiosis characterized by an excessive presence of bacteria in the small intestine. SIBO can lead to hormonal imbalances, constipation, weight gain, acne and other related issues.
Understanding Polycystic Ovary Syndrome
Polycystic ovary syndrome (PCOS) is a medical condition characterized by excessive production of androgens, which are male sex hormones typically found in small quantities in women. The term “polycystic ovary syndrome” is used to describe the presence of numerous small fluid-filled sacs (cysts) forming in the ovaries. However, it’s important to note that not all women with this condition have cysts, and conversely, some women without PCOS may develop ovarian cysts.
Ovulation is the process by which a mature egg is released from an ovary, usually with the intent of fertilization by male sperm. When fertilization does not occur, the egg is expelled from the body during menstruation.
In certain instances, women may experience a lack of ovulation. When ovulation is disrupted, the ovaries can develop multiple small cysts that produce androgens, leading to elevated androgen levels in women with PCOS. These hormonal imbalances often result in irregular menstrual cycles, excess hair growth and various PCOS symptoms.
The treatment of PCOS typically involves the use of medications. While it cannot provide a cure for PCOS, medication is employed to alleviate symptoms and reduce the risk of associated health complications.
The Link Between PCOS and Constipation
It is estimated that one out of every ten women is affected by Polycystic Ovary Syndrome (PCOS), a condition characterized by an imbalance in sex hormones that can lead to both reproductive and metabolic disruptions in women of childbearing age. Women with PCOS frequently report experiencing symptoms similar to those observed in individuals with Irritable Bowel Syndrome (IBS), such as sensations of abdominal bloating, constipation, diarrhea, as well as abdominal and pelvic discomfort.
Similar to PCOS, IBS is a complex disorder with multifaceted causes. Our understanding of IBS remains incomplete, but current research suggests that potential triggers may involve alterations in the composition of intestinal bacteria, known as the microbiota, or structural changes in stool consistency. These changes can be attributed to various factors, including persistent stress (both physical and psychological), post-traumatic stress disorder (PTSD), prolonged use of antibiotics, or a history of gastroenteritis.
Common Causes of Constipation
Absence of physical activity
Typically, individuals who engage in regular physical activity are less likely to experience constipation. Essentially, the colon responds positively to physical movement, emphasizing the importance of maintaining good muscle tone for regular bowel movements. Both the abdominal wall muscles and the diaphragm play vital roles in the defecation process. If these muscles are weak, they may not function effectively. However, it’s worth noting that while exercise can be beneficial, it may have a more pronounced impact on improving constipation in older individuals who tend to lead more sedentary lives compared to younger individuals.
Protection against chronic inflammation-related harm: Scientific research has highlighted that chronic, low-grade inflammation can evolve into a silent yet harmful force contributing to conditions like cardiovascular disease, cancer, type 2 diabetes and others. Here, you can discover straightforward strategies to combat inflammation and maintain overall health, as advised by experts from Harvard Medical School.
Opioid-induced constipation
The digestive system possesses receptors for opioids, and constipation can arise or worsen when individuals take opioid pain medications. Approximately 90% of cancer patients using opioids for pain management and 40% of those using opioids for chronic noncancer pain experience opioid-induced constipation.
Other medication-related factors: Constipation can be an adverse effect of numerous prescription and over-the-counter drugs. These include antacids containing aluminium, antispasmodics, antidepressants, tranquilisers, sedatives, bismuth salts, iron supplements, diuretics, anticholinergics, calcium channel blockers and anticonvulsants.
Irritable bowel syndrome (IBS)
Some individuals with IBS exhibit sluggish bowel movements, strain during defecation and abdominal discomfort. Constipation may represent the predominant symptom, or it may alternate with diarrhea, accompanied by cramping, gas and bloating.
Excessive use of laxatives
Laxatives are sometimes misused, particularly by individuals grappling with anorexia nervosa or bulimia. However, for those experiencing persistent constipation, long-term use of laxatives may be a reasonable solution. Modern formulations have reduced the likelihood of nerve cell damage in the colon and interference with its natural contractile abilities, which were concerns associated with older laxative formulations.
Life and routine changes
Factors such as travel disruptions to normal dietary and daily routines, the natural aging process affecting intestinal activity and muscle tone and hormonal shifts during pregnancy can all contribute to constipation.
Ignoring the urge
It is advisable to heed the call of nature promptly. Suppressing the urge to have a bowel movement, for any reason, can lead to constipation. Repeatedly disregarding these urges may eventually diminish the sensation.
Inadequate fibre and fluid intake
Diets low in fibre and fluids, coupled with high-fat consumption, can promote constipation. Fibre absorbs water, resulting in larger, softer stools that are easier to pass. While increasing fibre intake alleviates constipation for many, those with more severe cases may find that excessive fibre exacerbates their symptoms, causing gas and discomfort.
Other underlying causes
Various medical conditions can lead to constipation, including neurological disorders like Parkinson’s disease, spinal cord injury, stroke, or multiple sclerosis; metabolic and endocrine disorders such as hypothyroidism, diabetes or chronic kidney disease; bowel cancer; and diverticulitis. Additionally, systemic conditions like scleroderma can contribute to constipation. Intestinal obstructions stemming from scar tissue (adhesions) resulting from prior surgeries or strictures in the colon or rectum may compress, constrict, or narrow these areas, leading to constipation.
What Are the Symptoms?
Constipation can be identified by the following symptoms:
- Bowel movements occur less frequently than three times per week.
- Experiencing stool consistency characterized by lumpiness or hardness.
- Engaging in strenuous efforts during bowel movements.
- The sensation of an obstruction in the rectum, impeding the passage of stool.
- Perception of incomplete evacuation is the sensation that stool remains incompletely expelled from the rectum.
- Requiring assistance to empty the rectum, which may involve abdominal pressure applied with the hands or manual removal of stool from the rectum using a finger.
Helpful Tips for Managing Constipation
Implementing alterations in your daily regimen:
Initiating change in your daily routine can have a positive impact on alleviating constipation. Exercise and dietary changes are significant contributors to bowel habits. Commence by incorporating some physical activity into your daily life and introducing high-fibre foods.
Avoid making abrupt and drastic lifestyle modifications, as sustaining them long-term can be challenging. Instead, endeavour to gradually integrate a few of the following practices into your daily schedule to establish a beneficial routine:
- Establish regular meal times.
- Consume a glass of water immediately upon waking up.
- Consider incorporating bran cereal into your breakfast.
- Engage in light exercise, such as a walk, following your morning meal.
- Opt to park at a distance from your office, necessitating a brief walk to reach your destination.
- Dedicate a 20-minute walk to your lunch break.
- Experiment with new recipes featuring high-fibre ingredients like beans and legumes.
- Pack a piece of fruit to enjoy as a snack.
- Substitute white bread with whole wheat bread and white rice with brown rice.
- Ensure you get sufficient sleep.
- When you feel the urge to have a bowel movement, promptly utilize the restroom; refrain from holding it in.
- Allocate uninterrupted time daily for a bowel movement. Research suggests that individuals with regular bowel patterns tend to empty their bowels at roughly the same time daily.
- Keep a water bottle with you throughout the day.
- Consider enrolling in regular gym classes.
Incorporating a fibre supplement:
Fibre supplements, known as bulk-forming agents, function by increasing stool volume. This bulking effect prompts the bowels to contract, facilitating stool elimination.
Utilizing a fibre supplement is straightforward, and available in capsule, powder, gummy and chewable tablet forms. However, it is essential to consume an adequate amount of water alongside a fibre supplement, as failing to do so can exacerbate constipation.
Examples of fibre supplements include:
- Polycarbophil (FiberCon)
- Inulin (Fibre Choice)
- Wheat dextrin (Benefiber)
- Methylcellulose (Citrucel)
It’s crucial to stay well-hydrated while using a fibre supplement to avoid worsening constipation.
Increasing dietary fibre consumption:
An uncomplicated approach to alleviating constipation is to introduce more high-fibre foods into your diet. Dietary fibre comprises complex carbohydrates found in plant leaves, stems, whole grain bran, fruits, vegetables, nuts, seeds and grains. Notably, meat and dairy products contain negligible fibre content.
Commence this process by gradually augmenting your fibre intake. High-fibre foods include:
- Whole wheat bread
- Fruits like berries, apples, oranges, bananas, pears, raisins, figs and prunes
- Bran flakes and shredded wheat
- Popcorn
- Vegetables such as broccoli, spinach, sweet potatoes, carrots, squash, avocado and peas
- Beans and lentils
- Oatmeal
- Flaxseed
- Nuts
Opt for whole fruits over fruit juices, as juices lack fibre content. Additionally, increase your fluid intake to at least 1.5 litres per day along with a high-fibre diet.
Occasionally using a laxative:
Laxatives, while effective in the short term, are generally not a sustainable solution for addressing constipation issues. Prolonged and excessive use of certain laxatives can lead to serious side effects, including electrolyte imbalances and dehydration.
If you find it necessary to use a laxative periodically to alleviate constipation, it’s important to understand that not all laxatives are created equal, and some can be harsher than others. Here are various types of laxatives and their respective modes of action in alleviating constipation:
- Stool Softeners: These laxatives work by adding moisture to the stool, making it softer and easier to pass. Examples include docusate sodium.
- Osmotic Agents: Osmotic laxatives help retain fluid in the stool. Examples include magnesium preparations, polyethylene glycol, sodium phosphates and sorbitol.
- Stimulant Laxatives: These laxatives induce contractions in the intestines, facilitating stool movement. Examples include senna and bisacodyl.
Stimulant laxatives are the most aggressive, producing results within a few hours. However, they should not be used regularly, as prolonged use may disrupt normal bowel function. Dependency on laxatives for bowel movements can occur with long-term use, potentially leading to complications.
Preventive Measures
The encouraging news is that if you’re dealing with mild constipation, making straightforward adjustments to your lifestyle can effectively manage the condition. Here are some recommendations for prevention:
- Enhancing your fibre intake: Incorporate fibre-rich foods like fruits, vegetables and whole grains into your diet to promote better digestive function. If you experience bowel sensitivity, it’s advisable to steer clear of high-fructose fruits such as apples, pears and watermelon, as they can lead to gas.
- Increasing physical activity: Regular exercise contributes to the smooth passage of stool through the colon.
- Boosting your water consumption: Strive for a daily intake of eight glasses of water, while avoiding caffeine, which can have a dehydrating effect.
- Heeding your body’s signals: When you sense the urge to have a bowel movement, it’s essential to act promptly rather than postponing it.
How To Promote Healthy Bowel Movements
- Establish a consistent meal schedule by consuming your meals at the same predictable times each day. The digestive system operates most efficiently when it receives food at regular intervals. Maintaining regular meal timings can also promote a predictable pattern of bowel movements.
- Incorporate a high-fibre diet into your eating habits. Consume foods rich in both soluble and insoluble fibre. A diet encompassing whole wheat, oats, brown rice, fruits and vegetables can increase the volume of your stool and facilitate faster transit through the digestive tract. However, it’s advisable to gradually increase your fibre intake to avoid potential constipation.
- Integrate probiotics and prebiotics into your meals. Probiotics consist of foods containing beneficial live bacteria for your gut, including yoghurt, kimchi (a Korean dish comprising vegetables, garlic, ginger, chilli peppers, salt and fish sauce) and kefir (a fermented drink traditionally crafted from cow’s or goat’s milk). Prebiotic foods such as garlic, onions and bananas contain compounds that promote the growth or activity of probiotics. Probiotics and prebiotics stimulate the proliferation of gut bacteria and promote regular bowel movements.
- Maintain proper hydration by drinking ample water and decaffeinated beverages. Adequate water intake ensures that you remain well-hydrated. Water is a key component of stool, and increased water consumption can facilitate easier passage of bowel movements. Avoid caffeinated beverages like tea and coffee, as they can extract moisture from your stool, making it more difficult to have regular bowel movements.
- Engage in regular physical activity. Incorporating some form of daily exercise can stimulate the muscles in the lower portion of your digestive system and potentially encourage bowel movements. Exercise also helps prevent constipation by reducing the time it takes for food to traverse the large intestine.
Should you observe unusual patterns in your bowel movements that persist despite these lifestyle modifications, it is advisable to seek medical advice from a healthcare professional regarding your condition.
When To Seek Medical Attention
If efforts to increase fibre intake, engage in regular exercise and maintain proper hydration fail to alleviate the issue, your constipation might be classified as chronic. Depending on the underlying cause of chronic constipation, you may require physical therapy or even low-dose laxatives as part of the treatment plan.
In cases of chronic constipation, it is crucial to consult with a healthcare professional like a nutritionist, who can offer expert guidance on the most appropriate therapeutic approach. This becomes particularly significant if you exhibit any warning signs of an underlying medical condition, such as unexplained weight loss, rectal bleeding, or pain, or if your stools become consistently narrow and remain so.
All in all, if constipation or any other physical discomfort begins to disrupt your daily life, it is advisable to seek medical attention from a qualified healthcare provider.
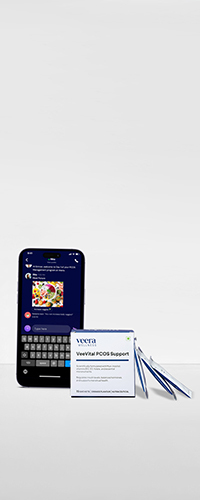
Learn More With Veera
Healthy gut health and proper bowel movement also contribute to weight loss which in turn helps manage PCOS. Experts at Veera Health value every aspect of your holistic health and not just some specific symptoms of PCOS. Veera Health offers judgment-free solutions to its patients and maintains utmost privacy so that you can share your problems without worrying.